How did I get involved in working with burnout? I got involved in working with burnout because at one time it was a very personal issue for me. My first experience with the emotional trauma physicians routinely witness occurred on the first night of my first clinical rotation as a third year medical student. I held the hand of a 19-year-old girl with terminal cancer while she died. I decided that unless I had more urgent clinical responsibilities, I would be with her, so she wouldn’t be alone in her final hours of life. I was told she was abandoned by her family. This was before palliative care was common. After she died, I had no idea of what to do with my subsequent emotional response. I didn’t even know how to name it. I just knew I was emotionally disturbed. I did what I saw the other medical school faculty model for me: I suppressed my emotions. I wanted to be “professional.” I was taught that the most important action, when presented with any clinical challenge, was to control myself, which meant suppressing any “unprofessional” emotions. I wanted to be professional, to be seen as competent and be accepted, and I learned rapidly.
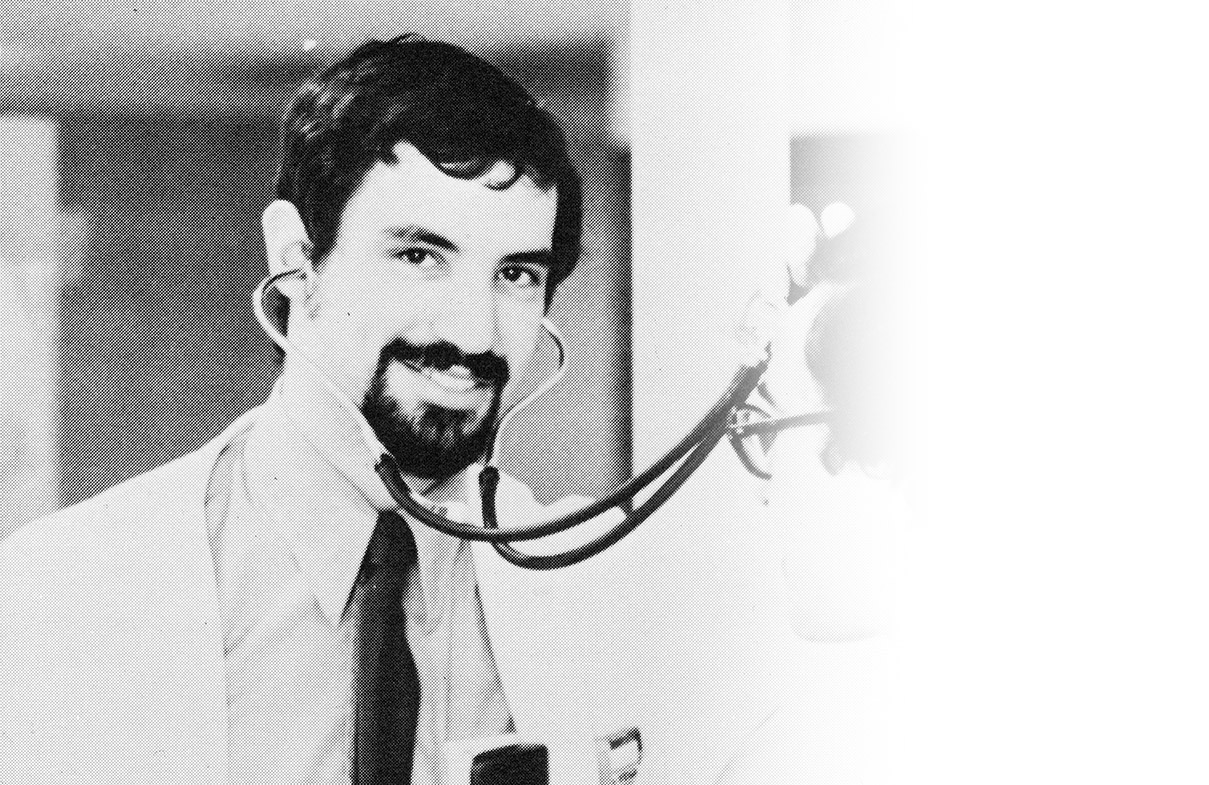
In my professional life I was an Emergency Medicine Physician, and the Medical Director of a Level II trauma center serving seven counties in an urban and rural setting. This was a high acuity emergency department, as 25% of the patients brought to us were admitted into the hospital. The hospital was the only locked psychiatric facility for the region and was also the local Poison Treatment Center. There was a constant stream of patients and their families with significant physical and emotional trauma 24 hours a day, seven days a week. At that time there was not much recognition of physician impairment, but I would see it in some physicians who turned to substance abuse–typically alcohol, but occasionally drugs–as a way of managing their reactions to their stressful work environments. My reaction was to work more, which numbed my experience of the negative emotions I didn’t know how to handle. I also started the first paramedic program in the area, serving as the project medical director and instructor. Additionally, I was clinical faculty at the Southern Illinois University School of Medicine, and taught family practice residents on rotation in the emergency department. I was also volunteer national faculty for Advanced Cardiac Life Support training programs for the American Heart Association, and active on the board of directors and as president of the Illinois chapter of the American College of Emergency Physicians. As you might already deduce, work was my addiction of choice.
As I’m writing this, it’s not surprising that the pace was not sustainable. At some point I realized I was exhibiting symptoms of what we now know is burnout. I was not particularly happy, the swing shifts were tolerable but difficult for my spouse, and I was emotionally pretty numb. I left Illinois and moved to a small town in Colorado to work full-time in the emergency department. Having only one full-time job was a significant reduction in working hours, and the absence of administrative and teaching responsibilities gave me ample free time. At the time, I didn’t know it, but one commonly adopted strategy to cope with burnout is to reduce work hours.
One of the first things I noticed was how much more fun I was having. However, this only lasted less than two years, and then my pattern of over-work and burnout started to return. Although working in a small Colorado mountain town emergency department was less intense than working in a major trauma center, every emergency room has its certain share of extreme trauma and patient interactions typical of an emergency department. When I picked up a book entitled “The Knife and Gun Club” in a Denver bookstore, I “recognized” myself in the pictures and stories written about the doctors, nurses, and paramedics who work in the emergency department of Denver General Hospital. When I looked at their photographs, I could see that same “look” in my own face when I looked in the mirror. They were feeling what I was feeling. They were experiencing what I was experiencing. I “woke up” to how much pain they (and I) were living with every day. Their description of depression, depersonalization, broken relationships, emotional numbness, and unhappiness was all too familiar to me.
I started to recognize that there was something about exposure to repetitive trauma (physical and emotional) that was debilitating to caregivers. But I still didn’t have a full understanding about how that could occur or what to do about it. I tried meditation, mindfulness practices, and even outdoor retreats, including a one-week backpacking trip designed for professionals experiencing burnout. While these attempts were temporarily useful, they really didn’t heal what I was experiencing. While I may have had some temporary relief and insights, these strategies really didn’t shift anything for me when I went back to work.
I didn’t really make any progress until I was involved in a head-on car crash when someone lost control on an icy road and skidded across the road as I was driving to work. My car was destroyed, and I sustained injuries that resulted in a permanent disability, along with chronic pain. I was physically unable to continue my practice of emergency medicine and sports medicine. The only thing I knew for sure was that taking narcotics for chronic pain was not an option for me. This was the event that propelled me into a process of learning how to heal both my burnout and the physical pain from the disabling injuries. I started a very personal study of mind-body interactions, and learned how to work effectively with my own emotions. Along the way I acquired both master’s and doctoral degrees in psychology. In learning how to heal myself, I also learned how to help others.
I realized that burnout in physicians, nurses, advanced practitioners and caregivers of all kinds was very often a consequence of small, repeated events that were perceived as traumatic. I called this “chronic PTSD.” (This is now starting to be recognized in the literature.) In the course of my doctoral studies I read about the discoveries of the neural mechanism (mirror neurons) that explains some of the emotional trauma experienced by caregivers. I also developed an educational approach to healing both burnout and emotional pain that has not only worked for me, it also has helped many other physicians, caregivers, and people whose lives were impacted by both physical and emotional trauma.